ARTS Program: Hyperbaric Oxygen Therapy for Children with Autism
What is Hyperbaric Oxygen Therapy?
Click Here to Read the Introduction to Hyperbaric Oxygen Therapy Transcript
But when our bodies don’t have the resources they need to complete all of these tasks, and when toxins or injuries or pathogens cause our to-do list to get longer and longer, disease and disability will begin to occur. And we can quickly go from happy and healthy to unhappy and unhealthy. In order to give the body more resources to heal and recover, there are many good nutrients that we can make sure we are getting by changing our diet and supplementing if necessary.
However, do you know which nutrient is most important of all? The answer is O2, or oxygen.
More than any food… more than even water itself… oxygen is the one nutrient that your body needs more than all others. Usually we don’t think of oxygen as a nutrient, but in reality, it is the most fundamental nutrient that we need for healing and for life itself.
So, how does hyperbaric oxygen help the body heal itself? The short answer is that hyperbaric oxygen gives the body more resources to do all the things on its to-do list. Hyperbaric Oxygen has been shown to:
- Destroy harmful bacteria
- Decrease inflammation
- Produce new collagen
- Increase white blood cells
- Regenerate bone
- Stimulate capillary growth
- Strengthen the immune system
- Help mitochondrial function
And perhaps most amazing of all, it even creates new stem cells in the body. After 40 sessions of hyperbaric oxygen, stem cell production increases all the way to 800%. Your body turns these stem cells into whatever cells that it needs, facilitating healing rapidly and naturally.
For more information about hyperbaric oxygen, or to schedule a consultation at the Oxford Recovery Center, please call 248-486-3636 or visit our website at www.OxfordRecoveryCenter.com.
What is the ARTS Hyperbaric Oxygen Therapy and how does it aid in Autism Recovery?
Based On Modern Research
 Oxford Recovery Center bases our usage of Hyperbaric Oxygen Therapy on the most modern research available in medicine. Our techniques customize the usage of hyperbarics based off of the needs of the patient.
Oxford Recovery Center bases our usage of Hyperbaric Oxygen Therapy on the most modern research available in medicine. Our techniques customize the usage of hyperbarics based off of the needs of the patient.
Attacks a Root Cause of Autistic Behavior

Studies have shown promising results by using Hyperbaric Oxygen Therapy to reduce the inflammatory symptoms associated with Autism in the brain and gastrointestinal system along with bringing actual healing to those damaged systems.
Highest Rated Medical Grade Equipment
 Not all Hyperbaric Oxygen Therapy chambers are created equal. Using the wrong types of chambers can in some cases lead to negative outcomes or lead to unsafe situations. Oxford uses only the highest quality Sechrist hard sided chambers to achieve optimal results.
Not all Hyperbaric Oxygen Therapy chambers are created equal. Using the wrong types of chambers can in some cases lead to negative outcomes or lead to unsafe situations. Oxford uses only the highest quality Sechrist hard sided chambers to achieve optimal results.
Synergistic by Design
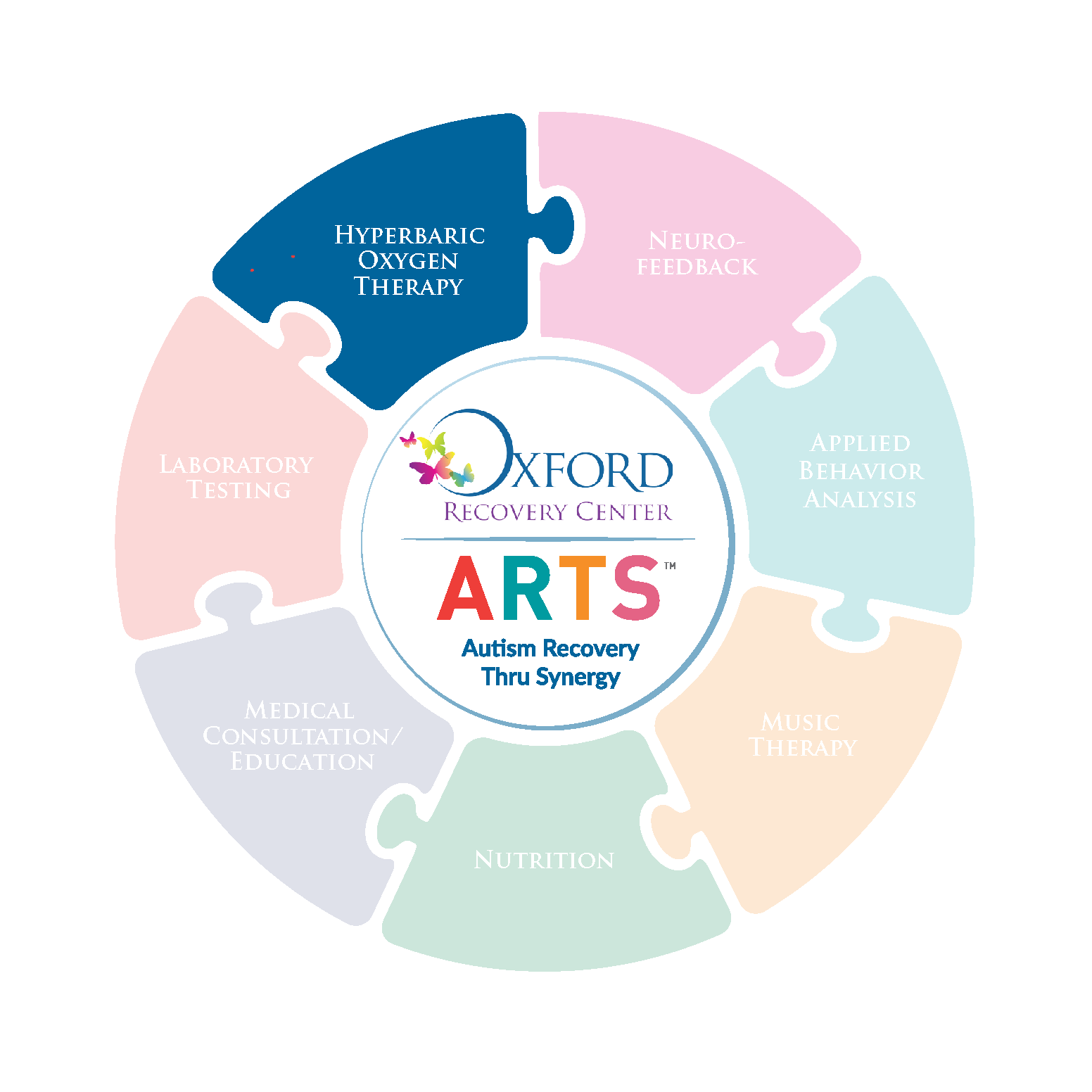
 Oxford’s ARTS nutrition program for children with Autism is designed to work synergistically with the other therapies offered in the Oxford ARTS program. With this approach, the ARTS program is able to accomplish a greater sum of results than each therapy would be able to achieve individually.
Oxford’s ARTS nutrition program for children with Autism is designed to work synergistically with the other therapies offered in the Oxford ARTS program. With this approach, the ARTS program is able to accomplish a greater sum of results than each therapy would be able to achieve individually.
Why does HBOT help children with ASD?
The exact reasons it helps children with ASD are still being researched, however, there are some clear correlations one can observe in the current research.
- First, it removes toxins, such as heavy metals from the body.
- It reduces inflammation allowing oxygen-deprived areas to have a return of blood flow.
- It builds new capillaries in the brain.
- It reduces the inflammation in the gut.
What do parents of children with ASD report?
Parents and doctors of autistic children have reported benefits of HBOT that included:
- Improved sleep
- Children becoming calmer and more affectionate
- Improved focus and attention
- Improved bowel function
- More “Present”
- Less Sensory Disturbance
- Improved Cognition
- More Language
- More “Connected” to Family
Hawaiian ASD study
Hawaii has more autism per capita than any other state.
An interesting fact, Hawaii, unlike other states, does not “regulate or restrict the amount of mercury-based preservative thimerosal used in immunizations.” (Markley, 2006)
One study done privately in Hawaii by Dr. Markley, protocol 20 hours HBOT at 1.5 ata with 100% oxygen, showed amazing results after just 20 hours, less than half the starting prescribed treatment.
All participants received comprehensive ADOS and ADI-R testing just prior to beginning HBOT. They also were evaluated using a Global Assessment of Functioning (GAF) scores.
The study consisted of 20 children, 4 female and 16 male.
The history of hyperbaric
Utilizing only the highest quality equipment
Hard vs Soft Sided HBOT Chambers
Why Treat Autism with Oxygen Therapy?

For Dr. Peterson’s Full Disretation click here: Children with Autism doing HBOT by Dr. Powell
Specific Aims
Eliminating the behaviors associated with children having autism would save this country millions of dollars and improve the lives of countless people. This, of course is not a tenable goal, but it is a testament to the financial burden directly related to autism. The Center for Disease Control estimates the lifetime cost to care for an individual with autism to be 3.2 million dollars. One in 100 children today is diagnosed with autism, with currently no treatment for this condition. Educating children with autism is being done through the public schools; however, treating the condition with hyperbaric oxygen therapy is showing positive results.
Medically
When studying peer reviewed research in autism, it is clearly a medical condition. A review of current literature will support the reason why medically hyperbaric oxygen therapy should be an avenue for treating autism.
Review of the Literature
Brain Research–Hypoperfusion
When a typical person focuses on a task or generates speech, the brain is doing more work and there is an increase perfusion with the blood flow to the brain. This increase in the blood flow to the brain supplies the brain with more oxygen and glucose, giving the cells their needed energy to perform their task. In autistic children, several studies have shown the opposite; these children actually have diminished blood flow to begin with, and when their brain is attempting to perform a task, such as generating speech or focusing, their blood flow does not increase giving them the needed oxygen and glucose the cells need. (Fox, 1986) (Muller, 1999) There is vasoconstriction instead of vasodilatation in the blood vessels. (Allen, 2003) This has been verified by studies that show an increase in p53 and a decrease in Bcl-2 in the brains of some children with autism. (Araghi-Niknam, 2003) Thus giving evidence for an indication of damage as a result of cerebral hypoxia (impaired oxygen delivery), resulting from the hypoperfusion. This is in correlation with the previously stated outcome of viral overload affecting the myelination process as a result of the ischemic effects from inflammatory process in which the vessels become inflamed and a downward spiral effects takes place resulting in cerebral hypoperfusion.
Cerebral hypoperfusion is simply decreased blood flow to the brain. There have been numerous studies in the medical literature demonstrating hypoperfusion in children with autism. “Bi-temporal hypoperfusion was confirmed in three independent groups of autistic children and provided the first robust evidence for localized dysfunction of the cerebral cortex in school-age children with primary autism.” (Boddaert, 2002) With newer upgraded brain-imaging cameras, detecting hypoperfusion in children with autism continues to become more defined. One way this has been documented is through the use of SPECT scans. One study conducted by Dr. James Wilcox in the Department of Psychiatry at Texas Tech University Health Sciences Center showed the hypoperfusion typically worsened with the age of the child, becoming “quite profound” in older children. The diminished blood flow can be seen with a clear correlation to many core autistic symptoms/behaviors. For example, when the Thalamus has hypoperfusion the results are repetitive, self-stimulatory, and unusual behaviors. When hypoperfusion is found in the temporal lobes the results are desire for sameness and social/communication impairments, or in the cingulate gyrus the outcome is manifested in difficulty recognizing familiar faces. Reduction on cerebral blood flow in the amygdale results in social deficits such as the ability to feel emotion and understand other’s emotions, and response to danger, and anxiety. (Ohnishi, 2000)
In order to look further into hypoperfusion, specifically in the temporal lobe, Zilbovicius and colleagues (2000) conducted a study using a PET scan. The advancements in PET scans allowed the researchers to look for abnormalities in regional cerebral blood flow (rCBF). The study consisted of twenty-one children with autism and ten non-autistic. Later, twelve more children with autism were added to the study. The children each had a PET scan and the image was reconstructed into 63 slices. The images were compared with t and Z statistics. The results revealed that the autistic group had significant hypoperfusion. There was no hypoperfusion in the comparison group. Regions with maximal hypoperfusion in the autistic group were centered in the left superior temporal gyrus, the right superior temporal gyrus, and in the right superior temporal sulcus (thought to process the human voice and coding facial expressions). These areas are involved in auditory processing. The left side generates an understanding of individual words; the right side deals with pitch, melody and sound intensity. When this study was redone on an additional 12 children with autism, the results were within millimeters of the initial study. They concluded there could be a correlation between the hypoperfusion and the deficits found in children with autism. The temporal lobe dysfunction is related to sensory abnormalities, thought also to be central to the processing information about the world around us. The right superior temporal sulcus hypoperfusion may reflect the difficulties for the children to respond to voices and/or read faces.
Critchley and colleagues published a study where they measured for changes in the cerebral blood flow when people with autistic disorder process facial expressions. Although high-functioning individuals with autistic disorder have normal to superior range of intelligence; they have abnormalities in social communication and emotional behavior that tends to not improve over time. The difficulty processing facial expressions of individuals with autism may be linked to the deficits in social behavior. The study used a Functional MRI (fMRI) to investigate brain activity in nine adults with autistic disorder and nine controls when consciously and unconsciously processing emotional facial expressions. The individuals all met clinical diagnosis for Asperger syndrome or autism using ICD-10. Subjects were shown pictures with different facial expressions, they then rated the emotion. Their research showed significant differences between the subjects with autism and the control group in processing facial expressions. More specifically this would stem from abnormalities in the medial temporal lobe, striatum and insula when processing facial emotions. This correlates with other studies that associate autism with cerebellar abnormalities. The amygdale (part of the brain that allows you to feel emotion and understand other’s emotions), part of the medial temporal lobe, is crucial to learning and representing the motivational meaning of stimuli. Critchley concluded that while these findings give clues to the difficulty for individuals with autism to process facial expressions, it is not clear as to the origin of the deficits. (Critchley, 2000)
Similiar to Critchley, Ohnishi and colleagues also reported reduced cerebral blood flow in people with autism. They addressed the problem of people with autism having impaired functioning in communication and social interaction, abnormal response to sensory stimuli, and desire for sameness that is obsessive in nature. They hypothesize that these areas of deficits may be associated with perfusion in the medial prefrontal cortex and anterior cingulated gyrus of the brain. The study consisted of twenty-three children with infantile autism and twenty-six non-autistic mentally retarded children who underwent SPECT scans (single photon emission computed tomography). Just prior to the scan each patient received an intravenous injection that allowed the researcher to examine the brain perfusion. The patients’ scores from the Childhood Autism Rating Scale (CARS) were compared with the areas of perfusion. The researchers discovered that there were decreases in regional cerebral blood flow in the patients with autism versus the non-autistic patients in the bilateral insula, superior temporal gyri, left inferior frontal gyrus, and left middle frontal gyrus. For the patients with autism there were no areas of increase in cerebral blood flow. There was also a positive correlation between the reduction in cerebral blood flow in the hippocampus (the area for short term memory and the area that regulates emotions—including the gyrus which is very sensitive to oxygen deprivation) and the amygdale, which is part of the limbic system (almond-shaped clumps of cells deep in the brain, deals with response to danger, anxiety, possible social interaction.) In conclusion, there was a reduction of cerebral blood flow in children with autism compared to the non-autistic population. These areas are related to the deficits found in children with autism, for example the left anterior cingulated gyrus is associated with communication and social interaction deficits. There is also some question as to the correlation with the amygdale and social deficits. People with frontal damage often show deficits related to the stereotypical and rigid behaviors often found in children with autism. These areas of reduced blood flow appear to be directly related to the deficits found in people with autism. (Ohnishi, 2000)
Another study linked the reduction in cerebral blood flow to damage in the cerebellum that is often found in people with autism. Muller et. al., conducted their study by doing PET scans on high-functioning adults with autism, with the premise that people with autism have deficits in language that according to former studies are directly related to deficits neurologically. With modern technology in brain imaging techniques, researchers can now study autism as a neurobiological disorder. Studies of normal adults show attention tasks activate the cerebellum; however, studies of patients with autism have shown the opposite. The researchers took five autistic adults and matched their gender matched with five controls. Cerebral blood flow was evaluated while subjects, autistic group versus control, were at rest, listening to tones, and listening to, repeating, and generating sentences using PET scans. The cerebral blood flow was evaluated on two elements, peaks and mean changes. They discovered that the subjects with autism showed reduced cerebellar activation during nonverbal auditory perception, suggesting cerebellar anomalies. This however was not related to motor activities, as the deficit was not shown during sentence repetition. The autistic population versus the control group also showed reduced activation during acoustic stimulation in the auditory cortex. The autistic group showed bilateral weaker activations in the superior temporal. They also showed an absence of activation in the middle temporal. However, in the left anterior cingulate gyrus (brodmann’s 24/32) there was an increase in activation that was not seen in the control group. They concluded that their findings suggest the autistic group may have deficits in language developed in the cerebellum region. The brain mapping suggested the dominance for language might be reversed or reduced. This might suggest early damage to areas of the brain, especially in the cerebellum. (Muller, 1999)
Brain Research–Inflammation
In 2005 John Hopkins University conducted a study on neurological conditions of autism by conducting autopsies on individuals with autism. They addressed the issue of people with autism having deficits in areas of communication, need for sameness, and social dysfunctions. These skills are directly related to specific areas of the brain. The question they sought to answer was, do those with autism have increased neuroinflammation in areas related to those deficits. They conducted autopsies and evaluated brain tissue from eleven people with autism for inflammation and tissue contents. The cerebrospinal fluid was also evaluated. The control group was seven patients with frozen tissue. They also collected cerebrospinal fluid from tissues of six living patients with autism. There was evidence of neuroinflammation, or inflammation of the brain. The results showed chronic neuroinflammation in the patients with autism. Vargas found the common trait of all the patients with autism was a chronic inflammatory process affecting both the brain and immune system functioning. The cerebellum showed considerable affects. It is not clear as to how the brain became affected, neurotoxins was one area considered. The researchers expressed they did not feel the inflammation did not occur exclusively during the prenatal development, rather ongoing chronic neuroinflammation involving both microglia and astroglia. (cells dealing with immune system and neurological tissues) They concluded that there is chronic neuroinflammation in patients with autism. They recommend “therapeutic interventions” dealing with the inflammation as a possible treatment for autism. (Vargas, 2005)
Neuroinflammation was also addressed as a possible result of enlarged activated astroglia. Aschner (1999) “observed swelling of astrocytes is associated with a nearly 50% decrease in the average capillary lumen as measured by electron microscopy, which will result in decreased blood flow because the flow of red blood cells is impeded.” Helt et al, brings that one step further to show the inflammation results in increasing difficulty in the body’s ability to eliminate waste products from the blood system, “hence impairing the cellular activities associated with neural activity and synchronization” (Helt et al 2008), correlating to Just and Castelli’s research. As a result, with time, different areas of the brain develop the inability to work together (Muller 2007). Once again, Helt stated, “If this inflammation could be controlled early in life, it might prevent such atypical development from taking place.”
Multiple studies have confirmed the neuroinflammation of children with autism. The inflammation in the brain causes edema, which increases the area between the cells, and therefore, could increase the amount of fluid inside the brain cells. Two studies confirmed this through a functional MRI (fMRI) (Hendry, 2006). The question with children affected by autism may not be if they demonstrate neuroinflammation, but why they have the inflammation.
Zerrate et al., addressed the issue of why the neuroinflammation by researching the link between the inflammation, behavioral abnormalities and Terbutaline, a preterm labor drug. The researchers hypothesized a correlation between prenatal drugs or chemical exposure could be a cause of autism. The study consisted of giving pregnant rats Terbutaline on selected days. After the pups were born, they were analyzed for behavior. Later they were anesthetized and the brains removed. The brains were then studied. The results demonstrated increased hyperactivity in the rats exposed to Terbutaline. There was also neuroinflammation. The most critical times of exposure were the second to third trimester of human brain development. They concluded a chemical exposure could affect the growing fetus in behavioral issue and neuroinflammation. This many contribute to the increase in the incidents of autism (Zerrate, 2007).
Herbert and Anderson (2008) suggest viruses or heavy metals infiltrating the body during early development as possible cause for neuroinflammation. The body’s inability to eliminate the virus overload or heavy metals from the body may stimulate an oxidative stress response which may lead to neuroinflammation, leading to deficits with brain synchronization. These early immunological insults to the brain may thus be core to the deficits seen in autism.
Brain Research—Synchronization
Some more resent research is taking the brain research a step further by looking at how the brain of the autistic child works in synchronization. Just, et al. (2004) looked specifically at the brain’s synchronization during a sentence comprehension task. They knew that high-functioning individuals with autism often display enhanced cognitive functioning with high vocabulary, yet they show a deficit in processing verbal instructions. The researchers hypothesized, “autistic participants may rely more on an enhanced word-processing ability (which would be indicated by more-than-normal activation in Wernicke’s area), and rely less on integrating processes that bring the words of a sentence together into an integrated syntactic and semantic structure (indicated by less-than-normal activation in Broca’s area.)” (Just, 2004) The researchers conducted the study with seventeen high-functioning autistic patients and seventeen normal participants. They were each given fMRI while asked questions that required sentence comprehension tasks. The participants were asked to press a button on either their right or left hand with the correct response to the question. Then the data was analyzed looking specifically at the left inferior frontal gyrus (LIFG) (Broca’s area) and the left superior and middle temporal gyrus (LSTG) (Wernicke’s area) and their synchronization. They discovered the autistic patients had a lower degree of synchronization between LIFG and the LSTG. The autistics showed less activation in the left inferior frontal gyrus versus the control group, however, they showed more activation in the left posterior superior temporal gyrus. The researchers concluded that the reduction in synchronization may give explanation for the deficits with auditory comprehension. The possible reason for this may be the autistic brain puts more emphasis on the individual words and details, with difficulty in higher-level abstraction, instead of comprehending the entire passage. The lack of synchronization may also account for social deficits in with the ability to integrate different types of information at abstract levels such as facial expressions, personal intent, and pragmatics (Just, 2004).
Another study conducted by Castelli, et at., intergraded synchronization with a reduction in cerebral blood flow. Again the research team looked at the functional deficits of a person with autism and compared it to the actual diagnostic deficits happening in the brain. They used a comparison study with ten adults diagnosed with autism and ten people in the control group made up of students and staff recruited from a university. The participants were shown twelve different brief animations, four different animations from three different types. After viewing, the subjects were questioned about what was happening in the animation. Their descriptions were coded in regards to “intentionality,” “appropriateness,” and “length.” Each subject underwent twelve scans, both PET and MRI, on the same day. The results were analyzed using software from the Wellcome Department of Cognitive Neurology in London, United Kingdom. The results demonstrated a direct comparison on the two groups there was a significant reduction in blood flow velocity in the autism subjects in the basal temporal area, superior temporal sulcus, and the medial prefrontal area. The extrastriate regions (brodmann’s 18/19) activated at the same rate; however, they were not interacting appropriately with the mentalizing network that showed a reduction. They concluded that people with autism do have impaired brain function with reduction in cerebral blood flow and lack of connectivity, especially evident when subject is mentalizing. One area of possible origin is the Amygdala (Castelli, 2002).
The pathophysiology of children with autism appears to include a number of different brain abnormalities. However, the area that is most often referred to as the site of the most abnormality is the cerebellum. The cerebellum damage shows consistent area for inflammation and also cell damage. One cell in particular is the Purkinje cell. Not only do multiple studies show a reduction in the Purkinje cell, but also Fatemi and colleagues have shown not only a reduction in the number of Purkinje neurons, but also a reduction in size (Fatemi, 2001). Chronic, ongoing process of neuroinflammation is a likely source for the reduction of the Purkinje Cells. Based on the research of Vargas and colleagues the findings of immune responses in the cerebellum were closely associated with degenerating Purkinje Cells, granule cells, and axons. In correlation to thimerosal, a side-effect of ethyl-mercury poisoning is reduction in the number of Purkinje Cells.
In summary as a relationship to hyperbaric oxygen therapy
Brain deficits in the area of hypoperfusion/decreased cerebral blood flow, reduction of the Purkinje cells, inflammation, and lack of synchronization is common research in the area of autism. These deficiencies are clearly linked to the deficits found in people with autism. Interestingly, neurological effects of mercury on the brain are in the amygdale, hippocampus, basal ganglia, cerebral cortex, damages Purkinje and granule cells in the cerebellum, paralleling the damage found in the autistic brain.
The neurological abnormalities manifest as deficits in cerebral blood flow, hypoperfusion, neuroinflammation, and lack of brain synchronization. This is important to understand in order to begin to find ways to treat people with autism, and understand the theory behind the treatment. This is reflective in the treatment of hyperbaric oxygen therapy. When a person receives hyperbaric oxygen therapy the blood flow in the brain is increased, and hypoxia and inflammation are reduced. Hence, it is reasonable to recognize how hyperbaric oxygen therapy may decrease neurological deficits and reduce symptoms of autism.
Benefits from hyperbaric oxygen therapy may not be limited to the child’s early years. In a study by Guy (2007) called “Reversal of neurological defects in a mouse model of Rett syndrome” he demonstrated reversing symptoms associated to Rett’s Syndrome was shown through biological treatment. The researchers activated MeCP2 in adult mice affected with Rett’s Syndrome. The results were phenotypic reversal of the syndrome. Guy et al. demonstrated defective neurons have the ability to be repaired into adulthood, contrary to popular belief of the damage being permanent after the “critical period.”
No matter the cause of the neuroinflammation the effects can be devastating. However, hyperbaric oxygen therapy may be one answer to addressing the neurological deficits in autism to be treatable.
Research Studies
Tami Powell Ph.D. Dissertation
Hyperbaric Oxygen Therapy For Children With Autism
- Hyperbaric oxygen therapy may improve symptoms in autistic children: Dr. Daniel Rossignol and Dr. Lanier Rossignol report that Hyperbaric oxygen therapy (HBOT) has been used with clinical success in several cerebral hypoperfusion syndromes including cerebral palsy, fetal alcohol syndrome, closed head injury, and stroke. HBOT can compensate for decreased blood flow by increasing the oxygen content of plasma and body tissues and can even normalize oxygen levels in ischemic tissue. In addition, animal studies have shown that HBOT has potent anti-inflammatory effects and reduces oxidative stress.
- Hyperbaric oxygen therapy might improve certain pathophysiological findings in autism: Dr. Daniel Rossignol’s findings suggest that numerous mechanisms of HBOT may have beneficial effects on the pathophysiology found in autism. These mechanisms include: increasing oxygen delivery to hypoperfused or hypoxic tissues, decreasing inflammation and oxidative stress, and increasing production of mitochondria and circulating stem cells. HBOT may also help children with autism by improving immune function, neurotransmitter abnormalities, and dysbiosis.
- Review of the Pathophysiology of Autism and Possible Benefits of Hyperbaric Oxygen Therapy (HBOT): After his third study on the use of HBOT in autism, Dr. Daniel Rossignol reported that many of the underlying pathophysiological findings may be ameliorable with HBOT, a therapy that is generally regarded as safe for children.
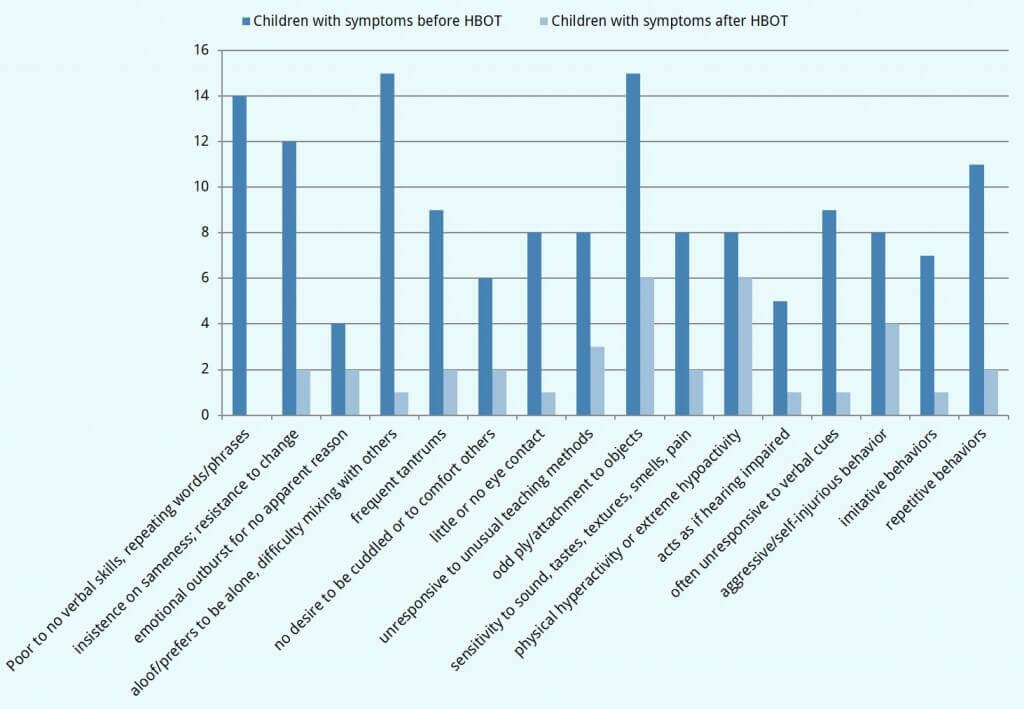
- Markley, M. Treating children with autism using hyperbaric oxygen therapy. Hyperbaric Medicine Center. 2007: The study found that children with autism who received hyperbaric therapy improved clinically in communications, social interaction, imagination/creativity, stereotyped behaviors, and global assessment of functioning (GAF) scores.
